Many pathology departments stand on the threshold of adopting digital pathology. The creation of an appealing business case for digital pathology is necessary to justify the acquisition of the new hardware and software and can be difficult to compile. This document guides you through the process of creating the business case.
Keep it simple
Before getting into costs and cost savings, I want to make something clear. I claim the biggest benefits of digitizing probably lies beyond the cost savings within the pathology department itself. Instead the bulk of gains will be health economically related and found in quality improvements throughout the entire cancer care chain, providing value for several care specialties and in the end increased value for patients. Although benefits such as reduced turnaround time shorter waiting times, increased diagnosis precision and faster treatments are obvious, they are very hard to monetize in a business case.
Having that said, presenting a more narrow economic model focusing on the increased efficiency and reduced costs for the pathology department itself is easier to quantify, and usually provide enough decision basis to justify the investment. By showing black numbers in such a model, one can argue that the investment is worthwhile since all the health economic benefits that will be realized throughout the cancer care pathway will add on top of that. Now, let’s look at an example of how a business case for a pathology department could be created.
Potential gains
Roughly, the gains of digitizing can be divided into 4 categories:
- Increased pathologist efficiency (review, workflow and internal consultations)
- Savings in external consultations
- Reduced cost of internal glass handling
- Real estate savings
Please note that the pathologist and secretary capacity gains described below are based on the assumptions that the pathology department can avoid future hiring within the organization required to “catch up” with the anticipated increase in the number of accessions and anticipated attrition. One could also argue that the increased efficiency enables the pathology department to handle more exams using existing resources.
Increased pathologist efficiency
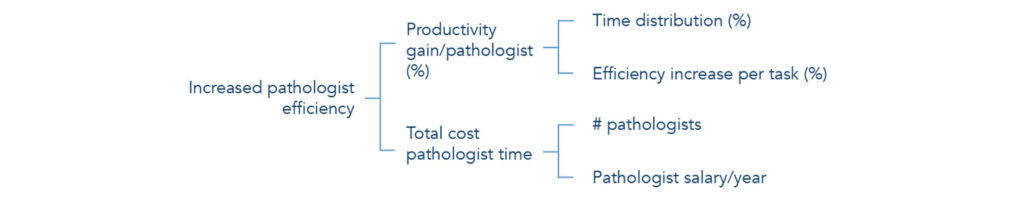
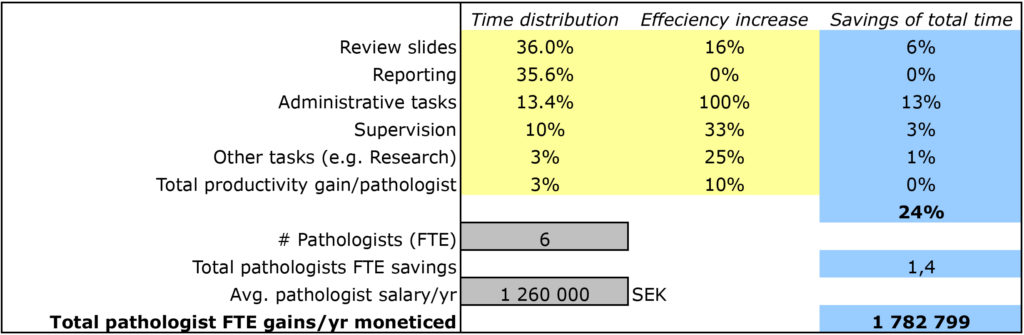
There is no doubt that an optimized viewing application for digital pathology will allow the pathologist to work faster compared to using a microscope. In order to calculate the potential capacity increase, one can start by dividing the daily work of one pathologist and estimate the effect that digitization will have on each component.
For instance built-in digital measurement tools, side-by-side comparisons and access to prior images will increase efficiency of slide review. Image analysis for mitosis and Ki67 counting and percentage cancer tissue calculations will, for example, remove the need for tedious, time-consuming tasks and also provide higher accuracy in diagnosis. In addition, tools for tagging cases for teaching and MDT during the actual review will also significantly reduce the preparation time for meetings. Another efficiency gain is to enable easier internal consultations where built-in chat and screen-sharing functionality can be used to quickly consult a colleague remotely instead of having to bring the glass to his/her room.
Summing up the efficiency gains for all components together will lead to an estimation of the total efficiency gain (X%). Also, multiplied by the organization’s total cost for pathologists, you will get a rough number of the value of the increased capacity. Basically, you calculate the cost saved to increase the number of reviewed cases by X% with the current staffing of pathologists.
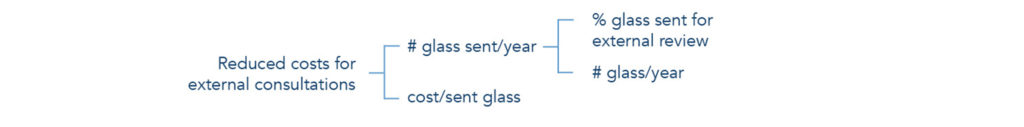
Savings in external consultations
The biggest saving for digitizing is probably the benefit of sharing digital images instead of sending physical glass. This will facilitate workload balancing, access to specialists and second opinion. Digital sharing results in shorter turnaround times, increased utilization of specialists leading to more accurate diagnoses, elimination of direct transportation and management cost of glass, as well as elimination of the risk for glass breakage or the glass getting lost.
Calculations can be very specific if the organization knows its costs associated with external consultations and sending glass. If these costs are unknown, one can simply assume that the same percentage of glass sent for consultations today will remain constant, and estimate the saved cost per glass by merely taking the glass logistics and management costs into consideration.
Reduced costs for internal glass handling
Digitization will lead to less glass management and administration for secretaries. Glass no longer needs to be sorted and handed to the right pathologists, and no previous cases need to be fetched from the glass archive. An estimation of the increased efficiency for secretaries could be made in a similar way as for the pathologists, but from experience, most pathology department managers have a rather good feeling for the potential savings, very often estimated in the number of FTEs saved.
For those afraid of the impact of the additional step of scanning, positive news is that most digital adopters agree that the savings in secretarial work significantly exceed the additional work of scanning.
Real estate savings
Light microscopes require the right environmental settings and often require the pathologist to work from the lab or hospital where the glass slides are produced. Digitizing pathology would mean that more pathologists could work from home or other locations, which potentially would provide opportunities to make savings related to real estate.
This is a sensitive question and probably disliked by some pathologists, but the fact is that the introduction of digital review opens up for remote review and also increased sharing of rooms. Since real estate is expensive and hospital floor space is scarce, savings can be realized by placing several review stations in the same room. However, implementing room-sharing is heavily dependent on the strength of cultural resistance towards room-sharing is within your organization. In radiology, for example, it is common practice to share rooms.

Figure 4. Example of how savings in rooms can be monetized. The cost per room and year is often available in the hospital’s annual report.
Costs
The direct costs of digitizing are easier to find out and can be divided into data storage, scanners, software for image viewing, distribution and management, and IT infrastructure.
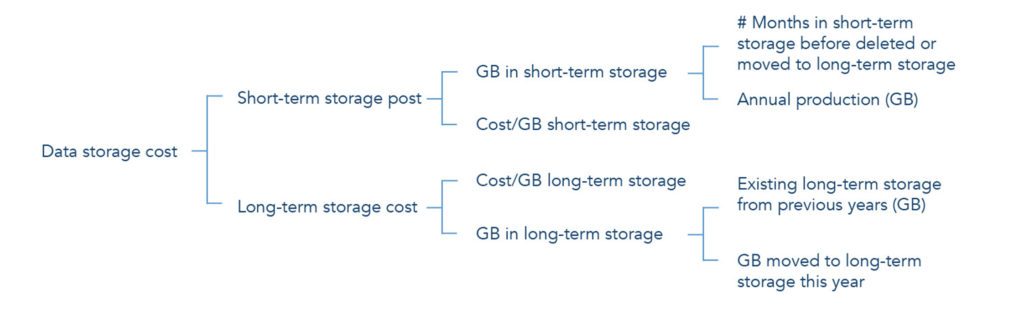
Data storage
Storing the large amounts of data that digital pathology images entails is probably the biggest challenge. Scanning magnification, the time and to what extent to store images will significantly affect the hardware sizing. The required redundancy, the performance requirements and the time for images in the short-term/long-term archive will heavily affect the cost per GB.
It is crucial that pathology departments decide on their storage strategy prior to estimating the total data storage cost for digital pathology images.
Scanners
Purchasing scanners is often one of the first steps when digitizing. These costs usually occur as a large upfront payment with annual service fee payments. It is important to consider the throughput of the scanners, so that they don’t become a bottleneck delaying the workflow, but can manage variable batch sizes and at the same time attain good image quality.
Software for image viewing, distribution and management
The software for image review, distribution and management fulfills a similar purpose to the PACS (Picture Archiving and Communication System) used in radiology, and plays a significant role in workflow effectiveness. The pathologist’s viewing component should be fast, intuitive, stable and easy to use in order to increase his or her efficiency. The PACS software should also be stable with a high uptime, and scalable to allow the digital volumes to grow without necessary forklift upgrades.
Costs for digital pathology software are often very transparent and follow a traditional license plus service fee model, or a pay-per-exam model.
IT infrastructure
The costs for IT infrastructure can be significantly high if an immature software solution is chosen, since this creates issues of incompatibility with other IT systems, the need for middleware and expensive integrations. To reduce this cost, it is important that the software solution mentioned above follows industry standards, such as HL7, DICOM and IHE, but also has a track-record of stability and successful integration with other IT systems across enterprises.
Conclusion—the return of investment
Based on the potential gains and the estimated costs, one can determine the return on investment for presentation to the hospital board of directors. Even if pessimistic estimations are used in calculations, you will normally gain a high ROI over a five-year horizon, and one thing that is certain is that there will always be someone in the room challenging your assumptions.
Your ROI is based on assumptions and will not be precise. However, even if only, say, 30% of the potential savings are realized, the investment will still be worthwhile, not to mention all the economic health benefits that will be realized on top of that.